Introduction

FUNCTION OF PANCREAS: The pancreas, a crucial yet often overlooked organ, plays a central role in maintaining the body’s overall metabolic balance and digestive health. While its contribution is not as widely recognized as that of the heart or brain, the pancreas is indispensable for functions that regulate blood sugar levels, digest food, and produce essential hormones. Understanding the pancreas’ anatomy, functions, and disorders is key to appreciating its critical role in maintaining homeostasis and promoting well-being.
In this comprehensive article, we will delve into the structure and function of the pancreas, exploring its dual role as both an endocrine and exocrine gland, the processes of digestion, blood sugar regulation, and the implications of pancreatic diseases such as diabetes and pancreatitis.
What is the Pancreas?
The pancreas is a vital organ located behind the stomach, nestled in the curve of the small intestine. It is approximately six inches long and shaped like a fish, with its head located near the duodenum (the first part of the small intestine) and its tail reaching toward the spleen. Although the pancreas is small compared to other organs, its roles in digestion and metabolic regulation are absolutely essential.
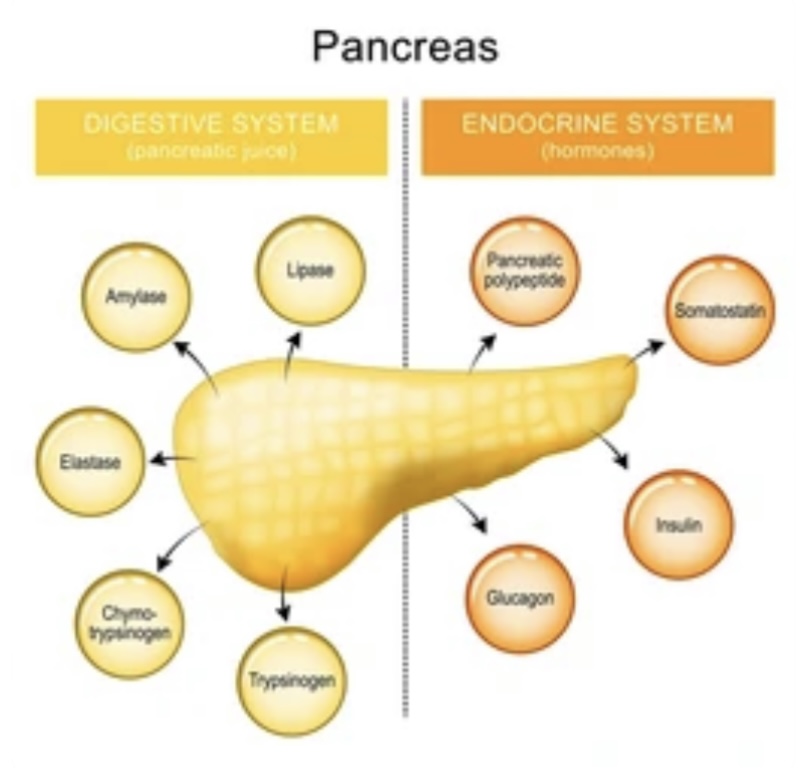
The pancreas has a dual role: it functions both as an endocrine and an exocrine gland. This unique structure allows it to release hormones directly into the bloodstream (endocrine function) and digestive enzymes through ducts into the intestines (exocrine function).
Overview of Pancreas Anatomy
The pancreas consists of specialized tissue that is divided into two main components:
- Endocrine Tissue (Islets of Langerhans): The endocrine component of the pancreas is made up of clusters of cells known as the Islets of Langerhans, which are responsible for secreting hormones into the bloodstream. These hormones regulate blood sugar and overall metabolic processes.
- Exocrine Tissue: The exocrine pancreas produces digestive enzymes and secretes them into the duodenum via the pancreatic duct. These enzymes break down food into its absorbable components.
Endocrine Function of the Pancreas
The pancreas plays a critical role in maintaining blood glucose levels within a narrow, optimal range. The hormone-secreting cells in the Islets of Langerhans produce various hormones that regulate metabolism and maintain energy balance.
Hormones Produced by the Pancreas
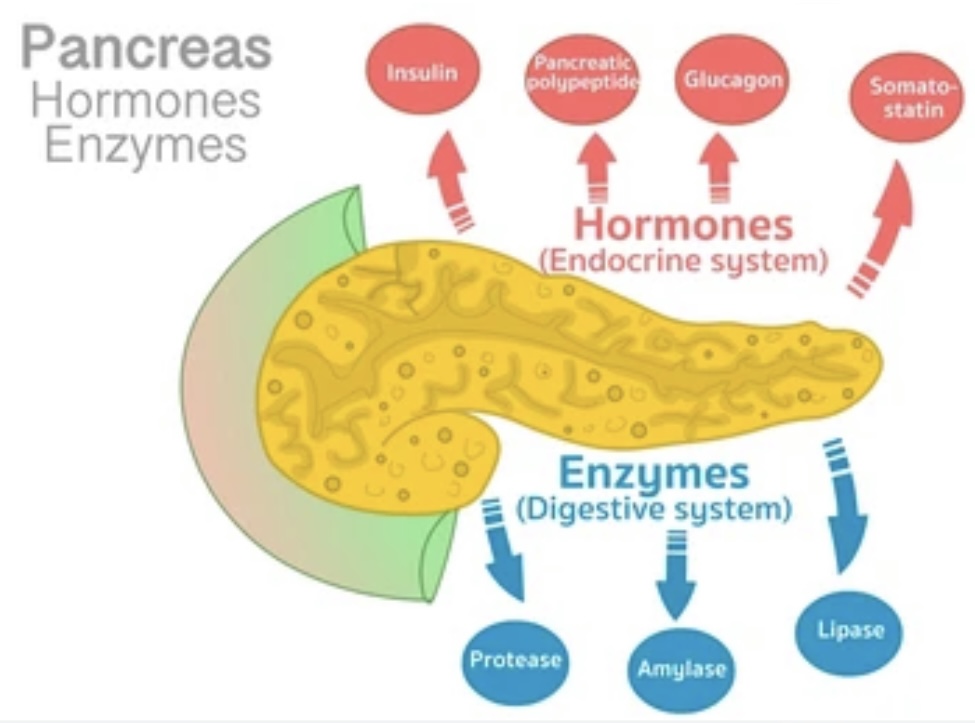
- Insulin: A hormone produced by beta cells in the Islets of Langerhans, insulin is critical for lowering blood glucose levels. It facilitates the uptake of glucose into cells, allowing for its use as energy or storage as glycogen in the liver and muscles.
- Glucagon: Produced by alpha cells, glucagon functions oppositely to insulin. When blood sugar levels are low, glucagon stimulates the liver to release stored glucose (glycogen) into the bloodstream, raising blood sugar levels.
- Somatostatin: Produced by delta cells, somatostatin inhibits the release of both insulin and glucagon, helping to regulate the balance between the two and prevent excessive fluctuations in blood glucose levels.
- Pancreatic Polypeptide: Secreted by the PP cells, pancreatic polypeptide is involved in the regulation of appetite, food intake, and the digestive processes.
Insulin and Its Role in Blood Sugar Regulation
Insulin plays a pivotal role in glucose homeostasis. After eating, glucose levels in the blood rise, prompting the pancreas to release insulin. Insulin acts like a “key” that allows glucose to enter cells where it can be used for energy. This mechanism is essential for maintaining normal blood glucose levels, and when the pancreas is unable to produce enough insulin (as in Type 1 Diabetes) or when the body becomes resistant to its effects (as in Type 2 Diabetes), blood sugar levels can become dangerously high.
Glucagon and the Counter-Regulation of Insulin
In situations where blood sugar levels drop, such as between meals or during exercise, the pancreas releases glucagon. Glucagon signals the liver to break down glycogen into glucose and release it into the bloodstream, thus raising blood sugar levels and providing the body with a steady supply of energy.
Other Hormones: Somatostatin, Pancreatic Polypeptide
- Somatostatin: This hormone has an inhibitory effect on both insulin and glucagon release, ensuring that blood glucose levels do not become too high or too low. It also regulates the digestive system by slowing down gastric emptying and inhibiting the secretion of gastrointestinal hormones.
- Pancreatic Polypeptide: Although its exact function is not entirely understood, pancreatic polypeptide is thought to regulate pancreatic secretion and contribute to appetite control.
Exocrine Function of the Pancreas
In addition to its endocrine role, the pancreas has a critical exocrine function related to digestion. It produces digestive enzymes that break down food components into absorbable molecules.
Digestive Enzymes: Amylase, Lipase, and Proteases
The pancreas secretes several key enzymes that aid in the digestion of carbohydrates, fats, and proteins:
- Amylase: This enzyme breaks down starches (complex carbohydrates) into simpler sugars like maltose. Amylase is important for the digestion of carbohydrates.
- Lipase: Lipase is responsible for breaking down fats (lipids) into fatty acids and glycerol, which are essential for energy storage and cell membrane formation.
- Proteases (Trypsin and Chymotrypsin): These enzymes are involved in the digestion of proteins, breaking them down into smaller peptides and amino acids that can be absorbed by the intestines.
Role of the Pancreatic Ducts
The exocrine cells of the pancreas secrete these enzymes into the pancreatic duct, which carries the enzymes into the duodenum (the first part of the small intestine) where digestion takes place. The pancreatic enzymes are activated once they enter the small intestine, helping to break down food so that nutrients can be absorbed by the intestines.
The Secretion of Bicarbonate
In addition to digestive enzymes, the pancreas also produces bicarbonate to neutralize stomach acid in the duodenum. This is crucial because the acidic contents from the stomach can damage the lining of the intestines, and the neutralization provides an optimal pH for digestive enzymes to function effectively.
Pancreatic Secretion Regulation
The secretion of digestive enzymes and hormones by the pancreas is tightly regulated by both nervous and hormonal signals.
The Role of the Autonomic Nervous System
The autonomic nervous system, particularly the parasympathetic branch, plays a key role in regulating pancreatic secretions. When food enters the stomach, the vagus nerve stimulates the pancreas to release digestive enzymes and bicarbonate.
Hormonal Regulation of Pancreatic Secretion
Several hormones also regulate pancreatic secretion. For instance:
- Cholecystokinin (CCK): Released by the small intestine when food enters, CCK stimulates the pancreas to secrete digestive enzymes.
- Secretin: Released when acidic food enters the duodenum, secretin stimulates the pancreas to release bicarbonate to neutralize stomach acid.
Pancreatic Health and Disorders
The pancreas can be affected by several diseases, ranging from inflammation to malignancy. Some of the most common disorders include:
Diabetes Mellitus (Type 1 and Type 2)
Type 1 Diabetes occurs when the immune system attacks and destroys the insulin-producing beta cells in the pancreas, leading to an absolute insulin deficiency. Type 2 Diabetes is characterized by insulin resistance, where the body’s cells do not respond properly to insulin, and beta cells may eventually become impaired.
Acute and Chronic Pancreatitis
Pancreatitis is the inflammation of the pancreas, often due to gallstones or excessive alcohol consumption. In acute pancreatitis, enzymes become activated within the pancreas itself, leading to self-digestion and inflammation. Chronic pancreatitis results in long-term damage to the pancreas and can lead to pancreatic insufficiency.
Pancreatic Cancer
Pancreatic cancer is one of the most aggressive forms of cancer, often diagnosed at advanced stages due to the lack of early symptoms. It primarily affects the exocrine tissue of the pancreas and can lead to obstructions, pain, and metabolic disturbances.
Cystic Fibrosis and the Pancreas
Cystic fibrosis is a genetic disorder that affects the production of thick mucus, leading to pancreatic duct blockages. This can result in pancreatic insufficiency, where the pancreas cannot secrete adequate digestive enzymes.
Pancreas in the Digestive Process
The pancreas is central to digestion. As food enters the small intestine, the pancreas releases digestive enzymes that break down proteins, fats, and carbohydrates. Without these enzymes, the body would be unable to properly absorb nutrients.
How the Pancreas Aids Digestion
In addition to its enzyme secretions, the pancreas plays a role in neutralizing stomach acid. This process ensures that the digestive enzymes from the pancreas are activated and that the small intestine functions properly.
The Pancreatic-Intestinal Axis: Interactions with the Gut
The pancreas is not an isolated organ; it interacts closely with the digestive system, particularly the intestines. Gut hormones, such as ghrelin, peptide YY, and GLP-1, help regulate the secretion of pancreatic enzymes and insulin, creating a pancreatic-intestinal axis. These hormones ensure that the pancreas is prepared to release enzymes when food enters the intestines.
Lifestyle Factors Impacting Pancreatic Health
Certain lifestyle factors can have a profound impact on pancreatic health:
Diet and Nutrition
A diet high in fats and sugars can strain the pancreas, leading to conditions like diabetes and pancreatitis. A balanced diet with adequate fiber, lean proteins, and healthy fats is essential for pancreatic health.
Alcohol Consumption and the Pancreas
Chronic alcohol consumption is a leading cause of pancreatitis, as it can cause inflammation and damage to pancreatic tissue.
Physical Activity and Pancreatic Health
Regular physical activity helps regulate insulin sensitivity, reducing the risk of Type 2 diabetes and improving pancreatic function.
The Role of Stress in Pancreatic Function
Chronic stress can alter hormone levels, affecting insulin secretion and potentially contributing to metabolic disorders like Type 2 diabetes.
Emerging Research and the Future of Pancreatic Health
Recent advances in stem cell therapy and regenerative medicine may one day offer solutions for restoring pancreatic function in individuals with diabetes or pancreatic insufficiency. Researchers are also exploring new treatments for pancreatic cancer and investigating how the pancreas can be regenerated after injury.
Conclusion
The pancreas is a multifunctional organ that plays a critical role in maintaining energy balance, digestion, and overall metabolic health. Its dual role as both an endocrine and exocrine gland allows it to regulate blood sugar, produce essential digestive enzymes, and maintain homeostasis within the body. Understanding the pancreas’ functions and disorders is crucial for preventing and managing diseases that impact this essential organ.
Reference Links:
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) – Pancreas
- Mayo Clinic – Pancreatic Diseases and Disorders
- American Diabetes Association – Pancreas and Diabetes
- PubMed – Pancreatic Function and Disorders
- American Cancer Society – Pancreatic Cancer
Discover more from ZOOLOGYTALKS
Subscribe to get the latest posts sent to your email.

