INTRODUCTION
Cells of immune system and the immune system protects multicellular organisms from pathogens attack.Highly adaptable, it defends the body against invaders as tiny as (~30 nm), intracellular virus that causes polio and as large as the giant parasitic kidney worm Dioctophyme renale.
These invading pathogens needs to be detected and destroyed using some specific mechanism. To accomplish this task, vertebrates have evolved a diverse and dynamic network of cells, molecules, and pathways.The functional immune system consists so many organs, molecules, cells, and pathways in such an interconnected and sometimes circular process.
A successful immune response to a pathogen depends interactions among diverse cell types :
- Innate immune cells that mount a first line of defense against pathogen,
- Antigen-presenting cells that communicate the infection to lymphoid cells, which coordinate the adaptive response and generate the memory cells, to prevent future infections.
All functionally specialized, mature blood cells (erythrocytes, granulocytes, macrophages, dendritic cells, and lymphocytes ) arise from a single cell type, the hematopoietic stem cell (HSC) .
The HSCs differentiate into mature blood cells by hematopoiesis.
Two primary lymphoid organs are:
- The bone marrow, where HSCs reside and give rise to all cell types.
- The thymus, where T cells complete their maturation.
CELLS OF IMMUNE SYSTEM
Cells of immune system arise from stem cells. HSCs are considered typical adult stem cells as they can differentiate into all types of blood cells.
Hematopoiesis: Lymphoid and myeloid progenitor cells arise from self-renewing hematopoietic stem cells. Hematopoietic stem cells have the ability to differentiate into many types of blood cells.
Hematopoiesis is the process by which hematopoietic stem cells develop into mature blood cells.
HSCs induced to differentiate (hematopoiesis) lose their ability to self-renew and make one of two broad lineage commitment decisions. It becomes the common myeloid erythroid progenitor (CMP), which produces all red blood cells (erythroid), granulocytes, monocytes, and macrophages (myeloid), or it becomes the common lymphoid progenitor (CLP) There is a possibility.
B-lymphocytes, T-lymphocytes, and NK cells develop from there. Myeloid cells and NK cells are members of the innate immune system and are the cells that first respond to infection and other attacks.
Lymphocytes are members of the adaptive immune response and generate sophisticated antigen-specific immune responses that evoke immune memory.
CELLS OF MYELOID LINEAGE
Cells of the myeloid lineage are the first responders to Infection cells that arise from a common myeloid progenitor (CMP).
It include red blood cells (erythroid cells) and various types of white blood cells (myeloid cells such as granulocytes, monocytes, macrophages, and some dendritic cells).
GRANULOCYTES
Granulocytes are at the first place in an immune response and are a part of the innate immune system.
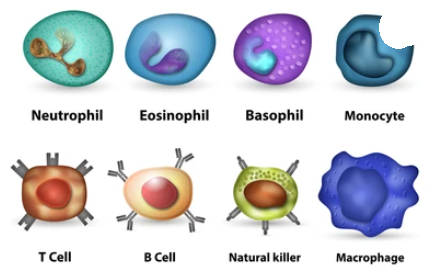
Granulocytes are white blood cells (leukocytes) that are classified as neutrophils, basophils, mast cells, or eosinophils.
All granulocytes have multilobed nuclei that make them visually distinctive and easily distinguishable from lymphocytes, whose nuclei are round.
NEUTROPHILS
Neutrophils constitute the majority (50% to 70%) of circulating leukocytes (see Figure 2-2a) and are much more numerous than eosinophils (1%–3%), basophils (1%), or mast cells (1%). After differentiation in the bone marrow, neutrophils are released into the peripheral blood and circulate for 7–10 hours before migrating to tissues, where they live only a few days. An increased number of circulating neutrophils, called leukocytosis, is used medically as an indicator of infection.
Neutrophils are the predominant first responders to infection and a major cellular component of pus that accumulates at the end of a short lifespan. Basophils are non-phagocytic granulocytes that contain large granules filled with basophilic proteins (i.e., they stain blue in standard H&E staining protocols).
BASOPHILS
Basophils are relatively rare in the circulation but can be very potent. Histamine, one of the most prominent proteins found in basophil granules, increases vascular permeability and smooth muscle activity. Like neutrophils, basophils may also secrete cytokines that modulate the adaptive immune response.
MAST CELLS
Mast cells are released from the bone marrow into the blood as undifferentiated cells; they mature only after they leave the blood. Mast cells are found in a variety of tissues, including the skin, connective tissue of various organs, respiratory, urogenital, and mucosal epithelial tissues of the gastrointestinal tract. Mast cells plays an important role in the development of allergies.
EOSINOPHILS
Similar to neutrophils, eosinophils are mobile phagocytic cells that can migrate from the blood into tissue spaces. Eosinophils and neutrophils play their most important role in the defense against multicellular parasitic organisms, including worms. Like neutrophils and basophils, eosinophils may also secrete cytokines that regulate B and T lymphocytes, thereby influencing the adaptive immune response. Eosinophils are better appreciated as contributors to asthma and allergy symptoms.
MYELOID ANTIGEN-PRESENTING CELLS
A group of phagocytic cells (monocytes, macrophages, dendritic cells) with professional antigen-presenting cell function (APC) also arise from myeloid progenitors.
Myeloid APCs are considered a cellular bridge between the innate and adaptive immune system, as they encounter pathogens at sites of infection and relay this encounter to T lymphocytes in lymph nodes.
Myeloid APCs are considered a cellular bridge between the innate and adaptive immune system, as they encounter pathogens at sites of infection and communicate this encounter to T lymphocytes in lymph nodes (“antigen presentation”).
Each APC responds to pathogens by secreting proteins that attract and activate other immune cells.
MONOCYTES
Monocytes are a heterogeneous population of cells that make up approximately 5% to 10% of white blood cells, migrate into tissues and differentiate into a variety of tissue-resident phagocytes, including macrophages and dendritic cells.
During hematopoiesis in the bone marrow, granulocyte-monocyte progenitors differentiate into pro-monocytes, leave the bone marrow and enter the blood, where they further differentiate into mature monocytes.
Monocytes that migrate into tissues in response to infection can differentiate into specific tissue macrophages. Some macrophages are long-term residents of tissues and play an important role in regulating repair and regeneration..
DENDRITIC CELLS
Dendritic cells are so named because they are essential for the initiation of immune responses and are covered with long membranous processes that resemble the dendrites of neurons and dynamically expand and contract.
Dendritic cells perform distinct functions of antigen capture at one site and antigen presentation at another site.
Outside the lymph nodes, immature forms of these cells monitor the body for signs of invasion by pathogens and capture invading or foreign antigens.
After they process these antigens, they migrate to lymph nodes where they present the antigen to naive T cells to initiate an adaptive immune response.
ERYTHROID CELLS
Cells of the erythroid lineage (red blood cells, or erythrocytes) also arise from common myeloid progenitors (sometimes called common myeloid-erythroid progenitors). They contain high concentrations of hemoglobin, circulate in blood vessels and capillaries, and deliver oxygen to surrounding cells and tissues. Damaged red blood cells release signals (free radicals) that trigger innate immune activity.
MEGAKARYOCYTES
Megakaryocytes are large myeloid cells found in the bone marrow that circulate in the blood and give rise to thousands of platelets, small cells (or cell fragments) that are involved in clot formation. Platelets share some characteristics of independent cells but do not have their own nucleus.
LYMPHOID LINEAGE
Cells of the Lymphoid Lineage Regulate the Adaptive Immune Response Lymphocytes are major cellular players in the adaptive immune response. They make up 20-40% of circulating white blood cells and 99% of cells in the lymph.
Lymphocytes can be broadly divided into three major populations based on functional and phenotypic differences: B lymphocytes (B cells), T lymphocytes (T cells), and natural killer cells (NK).
Notably, T cells and B cells look identical under the microscope. Therefore, in order to distinguish the subpopulations of lymphocytes in which each B or T cell also expresses antigen-specific receptors (B-cell receptor (BCR) and T-cell receptor (TCR)), the surface proteins they express depends heavily on the characteristics of :
B-LYMPHOCYTES

B-lymphocytes (B cells) is a letter designation derived from where they mature in the bursa of Fabricius in birds. The name turned out to be apt because the bone marrow is the major site of maturation in humans, mice, and many other mammals.
Mature B cells produce membrane-bound immunoglobulin (antibody) molecules that bind antigens. It clearly differs from other lymphocytes and all other cells in the synthesis and presentation of the B-cell receptor (BCR).
T-LYMPHOCYTES

T lymphocytes (T cells) get their letter designation from where they mature in the thymus. Like B cells, T cells express their own antigen-binding receptors called T cell receptors. However, unlike membrane-bound antibodies on B cells, which can recognize soluble or particulate antigens, T-cell receptors recognize antigens (usually peptide) only recognizes the processed part.
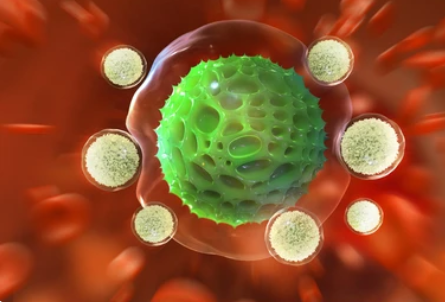
NATURAL KILLER CELLS
Natural killer (NK) cells are lymphocytes closely related to B and T cells. They are characterized by the expression of a surface marker known as NK1.1 and the presence of cytotoxic granules.
NK cells also express receptors for immunoglobulins and thus can self-decorate with antibodies that bind pathogens or pathogen proteins on the surface of infected cells. This allows NK cells to bind to a variety of target cells (regardless of their MHC class I expression).
When antibodies bring NK cells into contact with target cells, the NK cells release granules and induce cell death.
NKT CELLS
Another cell type of the lymphoid lineage, NKT cells, has recently received much attention and shares features with both conventional T lymphocytes and NK cells.
Like T cells, NKT cells have a T cell receptor (TCR) and some express CD4. However, unlike most T cells, NKT cell TCRs are less diverse, recognizing specific lipids and glycolipids presented by MHC protein-associated molecules known as CD1. Like their innate immune relatives, NK cells, NKT cells have antibody receptors and other receptors classically associated with NK cells.
Activated NKT cells may release cytotoxic granules that kill target cells, but may also release large amounts of cytokines that can enhance and suppress immune responses. They appear to be involved in human asthma, but they can also inhibit autoimmunity and cancer development. Understanding the precise role of NKT cells in immunity is a research priority.
CONCLUSION
Immune system in vertebrates involves a network of cells, molecules, organs, and pathways in such an interconnected process.
Cells of immune system arise from Hematopoietic stem cells (HSC’s). By the process called Hematopoiesis.
Cells of immune system consists of cells of myeloid lineage (granulocytes), Myeloid antigen presenting cells (monocytes, macrophages, erythroid cells and dendritic cells), and lymphoid lineage cells (B&T Lymphocytes, NK cells and NKT cells). They all function in a synchronized manner to fight against foreign material or a pathogen (also known as immune response).
Discover more from ZOOLOGYTALKS
Subscribe to get the latest posts sent to your email.

